
Understanding ‘mets’
When we talk about cancer, we use stages to determine where the cancer cells have traveled. When I was first told that I had cancer, the doctor said I had a tumour in my bowel and the cancer had traveled to my liver and maybe my lung (can’t remember which one now and it hadn’t, thank goodness) so bascially my cancer had mestastasized, quite simply put, it had spread from the primary source (my bowel/colon) through lymphatic nodes and to other organs. So, when people with cancer talk about mets (also known as lesions) or in my case liver mets, they are saying a form of tumour in another organ. I didn’t have liver cancer, I had mestastasized stage 4 bowel/colon cancer. I am going to focus on stage 4 cancer, as that is what I had.
 The reason that I am writing about this as when I was first diagnosed, I didn’t have a clue about what any of my doctors were talking about. It was hard enough to wrap my head around having cancer. Then they add stage four into the mix; I made the mistake of Googling – DO NOT DO THAT! Then, they were talking about liver mets. It is quite frankly, far too much to handle at once. So if you are newly diagnosed, I hope this can offer some relief, many people may already know about these things, so if you are one of them, no need to read I guess! Another reason, I want to write this post is for people who know someone with cancer, I am sure it can get very confusing for you and the last thing you want yo do is bombard an already bombarded person with more questions! You get my point…..
The reason that I am writing about this as when I was first diagnosed, I didn’t have a clue about what any of my doctors were talking about. It was hard enough to wrap my head around having cancer. Then they add stage four into the mix; I made the mistake of Googling – DO NOT DO THAT! Then, they were talking about liver mets. It is quite frankly, far too much to handle at once. So if you are newly diagnosed, I hope this can offer some relief, many people may already know about these things, so if you are one of them, no need to read I guess! Another reason, I want to write this post is for people who know someone with cancer, I am sure it can get very confusing for you and the last thing you want yo do is bombard an already bombarded person with more questions! You get my point…..
It was only recently that I found out there are sub-categories within stage 4, I saw a post on Instagram. Here they are listed below:
‘Stage IV: In Stage IV, colon cancer is divided into stages IVA, IVB, and IVC. The cancer has spread outside of the colon and has been carried through the lymph and blood systems to distant parts of the body, this is known as metastasis. The most likely organs to develop metastasis from colorectal cancer are the lungs and liver.
- Stage IVA: Cancer has spread to one area or organ that is not near the colon, such as the liver, lung, ovary, or a distant lymph node.
- Stage IVB: Cancer has spread to more than one area or organ that is not near the colon, such as the liver, lung, ovary, or a distant lymph node.
- Stage IVC: Cancer has spread to the tissue that lines the wall of the abdomen and may have spread to other areas or organs.’
This information and below image was taken from the Colorectal Alliance.
**TRIGGER WARNING** I have inserted medical images of my liver and post surgery incision (with staples/clips), so if you do not want to see this – stop reading now!
There are many variable factors for each person and their diagnosis, how you respond to treatments (chemotherapy and radiation) and how long you’ll need to stay on them, the size and location of mets and whether surgery is an option. A biopsy will determine what gene type your cancer is (I am RAF – WILD type) and the grade, The World Health Organisation has a grading system, (low/high grades, mine is a low grade). I cannot see into the future (for anyone including myself) but what I do know is that everyone is unique. Neither I nor you are a statistic and I for one do not research stats. (well apart from that one time on diagnosis day), I fucking hate those five year timelines, saying this % will/won’t live until bla, bla,bla and I will always politely tell anyone that brings it up, not to talk to me about statisitics. Of course, we have to keep it real but we also NEED HOPE (which is initally zapped right out of us when we hear those words), looking at statistics will just drain the life out of us more.
Many people with stage 4 cancer are on chemotherapy for life; Yvette was first diagnosed with stage 1 rectal cancer in 2014 (aged 41), then in February 2018, after a long battle to be heard, she was diagnosed with stage 4 (IVC) rectal cancer with mets to her liver, ovary, retro peritoneal and peritoneal cavity. Yvette has Folfiri chemotherapy and Avastin fortnightly and has a chemo pump at home for another 46 hours (slow release chemotherapy) with the hope of having her tumours removed in the future, plus scans every three months to monitor her cancer.
Yvette said, “Praying it works for as long as it can. Trying to live life between chemo weeks and scans.” Yvette explained to me that she does what she has to, to be there for her youngest daughter, she also has two adult children. I will be sharing Yvette’s full story soon.
I was in the category of stage 4 (IVA) I had a primary tumour in my sigmoid colon which was removed with clear margins (15cm in total) I did not require an ostomy bag. There are many, many people who do have surgery and require an ostomy bag (my mum had one), some may later have surgery to reverse it. After my diagnosis, my surgeon went straight in and removed the primary tumour from the bowel as well as several lymph nodes. She described (and drew) it as a piece of pie, due to the location of the cancerous lymph nodes. My bowel was 90% blocked so surgery was imperative. Many people may start with chemotherapy then surgery, like I said, we are all different.
I followed surgery with six months of chemotherapy Fluorouracil (5 FU) and Oxaliwin. Adam Nosworthy, my oncologist used CT/MRI scans to monitor my ‘mets’ and in my case he told me that the potential met on my lung was in fact scar tissue and not malignant and that I also had several mets on my liver. I completed all chemotherapy (it sounds so easy on paper) which was horrendous, not going to lie, I hated it but I havd a very good clinical repsonse to chemo. I had my final chemo 17th April 2020. By May 2020, my onc told me that the liver mets appeared to be calcified (in his words – ‘like scar tissue and most likely not cancerous anymore’) and to come back in three months.
So, that is what I did. Three months later, I did bloods, saw my oncologist 14th August 2020, CEA markers had shot up to 22.8 ng/ml. An MRI on 17th August 2020 showed that the mets had never really calcified and that the cancer was still there and had been growing, which caused my tumour (CEA) markers to increase (the cancer rollercoaster). Remember, scans are NOT 100%!
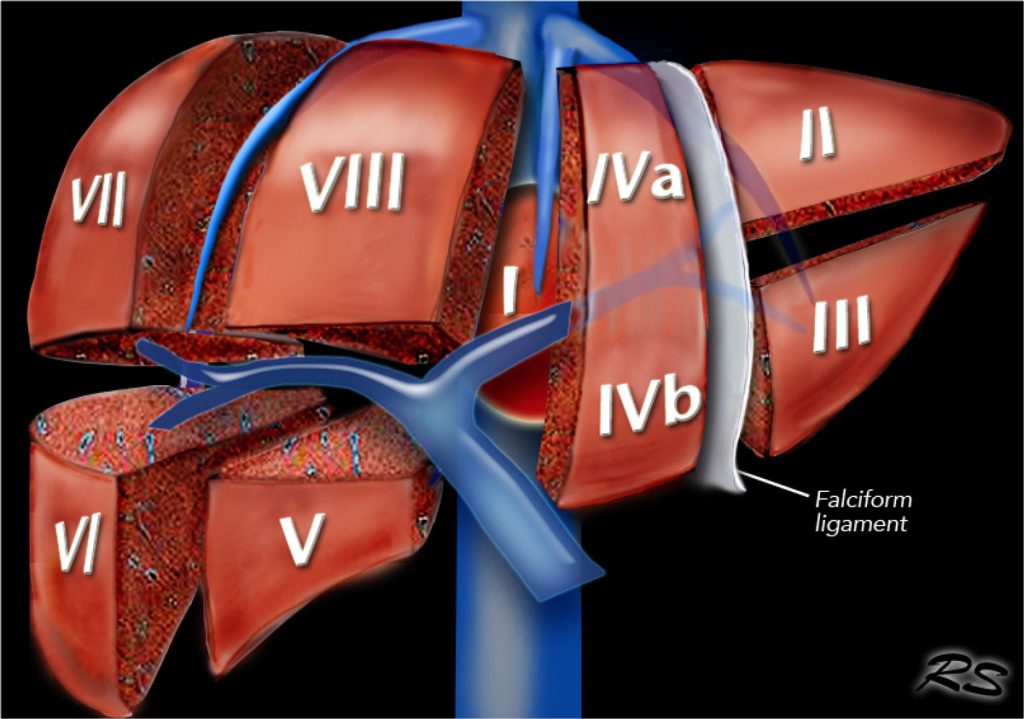
I was referred to Professor Ramos and we (Damian and myself) had our first meet on Friday 21st August, he brought up my scan on his computer and explained that there were lesions on the the right lobe, he would remove the entire lobe and gall bladder and he drew them on a picture of the digestive system (he has a note pad of them so the patient can take away) it was comforting to visualise what he would be doing. He further explained that he would have to remove part of the left lobe and those lesions there. Initially, I think we were told I had six lesions across the liver. We were also told that he would use a sonar device to check my stomach and surrounding areas for any other tumours, if he did find any then he would be unable to operate. Prof did also say it was highly unlikely to find further tumours and his hope was to operate and give me a ‘long and happy life’! Despite his positivity, all we heard was the ‘if we find more’ and that was a heart sinker, just when you think you know so much about a subject, you are thrown a curve ball, but we did our best to stay positive and his kind words became a mantra that we still use today. ‘I will live a long and happy life’. The surgery would take around four hours and he offered to do it on Monday 24th, which meant just waiting the weekend with the uncertainty of what he had just told us. If not that day, it would have to be the following Monday, after chatting with family, we booked the surgery for the 24th, get the job done.
on a picture of the digestive system (he has a note pad of them so the patient can take away) it was comforting to visualise what he would be doing. He further explained that he would have to remove part of the left lobe and those lesions there. Initially, I think we were told I had six lesions across the liver. We were also told that he would use a sonar device to check my stomach and surrounding areas for any other tumours, if he did find any then he would be unable to operate. Prof did also say it was highly unlikely to find further tumours and his hope was to operate and give me a ‘long and happy life’! Despite his positivity, all we heard was the ‘if we find more’ and that was a heart sinker, just when you think you know so much about a subject, you are thrown a curve ball, but we did our best to stay positive and his kind words became a mantra that we still use today. ‘I will live a long and happy life’. The surgery would take around four hours and he offered to do it on Monday 24th, which meant just waiting the weekend with the uncertainty of what he had just told us. If not that day, it would have to be the following Monday, after chatting with family, we booked the surgery for the 24th, get the job done.
While operating, Prof. Ramos found more lesions that had not been visible on the scan, which further proves that they are not 100% reliable. Luckily, he was able to remove them all and he took 70% of my liver and gall bladder as mentioned earlier. The surgery actually lasted six hours but it was a success!
**TRIGGER WARNING** I have inserted medical images of my liver, so if you do not want to see cut-out pieces of my old diseased liver – stop reading now!
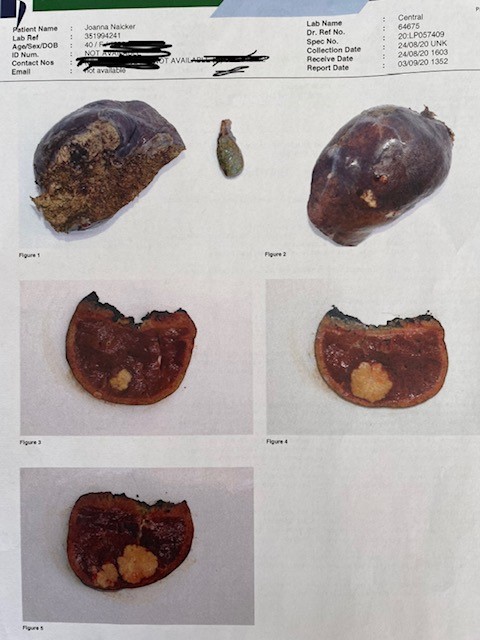
I often used to think, what does a met/lesion look like?! I used to imagine some floaty thing and I always worried about how a surgeon can cut them out with clear margins! I was quite surprised when I saw photos of them in my pathology reports. I have lifted snippets of my histology below:
HISTOLOGY
Specimen 1 – “Extended right hepatectomy and gall bladder” consists of a liver lobe weighing 659.6g and measuring 154 x 134 x 66mm. The largest tumour measures 35mm in maximal dimension. With an extension to reove segmant 4a.
Specimen 2 – liver segment 3 posterier & Specimen 3 – liver segment 3 both showing involvement by foci of metastatic adenocarcinoma.
Specimen 4 – liver segment 4B showing involvement by foci of metastatic adenocarninoma.
The right lobe consists of segments 5, 6, 7 and 8. I also had segments 3, 4a and 4b removed.
The point is those yellow parts are where the cancer had spread. If you look, I was SO LUCKY to catch this when I did. I cannot say it enough, BE YOUR OWN HEALTH ADVOCATE!
It took me many months whilst I was in the UK to be heard and by the time I finally had a CT (thanks to a trainee GP who listened to me and sent tests off, which prompted the CT), I was nearing moving to South Africa. I was eventually given my CT results and diagnosis over the phone as I had already relocated to Johannesburg. Not the best news to get over the phone but nonetheless, we could start the healing process. I was and still am blessed to have the best medical teams looking after me. Without these professionals, I would not be sitting here writing this today.
When I saw these images in my folder of papers and reports, I realised how close the cancer was to breaching the liver and traveling further. But, also that the human body is incredible. I had 70% of my liver removed and in my surgeon’s words I ‘was at significant risk of post-operative liver dysfunction and possibly even liver failure’ (glad I found his report later haha) ‘It is however, anticipated that her remnant liver should cope until hypertrophy occurs. She may require a longer time in ICU than usual should there be progressive liver dysfunction.’

I was in ICU for three days and in hospital for a total of six days. Regenerating such a large part of your liver is tiring, to say the least but it grew back and my most recent bloods show a fully functioning, healthy liver. Our bodies are insane and can do things beyond our imaginations. I also strongly believe in the body’s intuition to heal, and I have done a huge mental and physical overhaul these last couple of years. Most recently, changing my diet and you all know how I promote exercise, finding balance, enjoying everyday and keeping life simple. I can’t control so many things in my life, so I do my best to just LET IT GO……there will always be bad days, which is why the good days are the most important – my feature photo is an example of a good day!
I hope this has been informative for anyone in a similar situation and well, just for anyone interested in learning more. Please always remember, there are people out there, that have not been as lucky. Let us ALL (not just people who have had or still have cancer) enjoy this life for them. I have lost many friends along the way that didn’t deserve to die, as well as my beautiful mother. Let’s keeping telling their stories and our own to prevent any unnecessary suffering. If you have any symptoms, please see your doctor. You are never too young and early screenings save lives!
Love Jojo xoxo
Ps. If you have any more questions about liver surgery, please don’t hesiate to email me…I have long reports which I can’t add to a short blog!

